Information for Providers
Many adult survivors of childhood cancer feel fertility preservation and the ability to have a future family are important. Understanding there may be fertility preservation options available and referring children and their parents in a timely manner to reproductive specialists can improve their future quality of life.
Introduction
Parents may not be aware there are options for preserving fertility in their child diagnosed with cancer. However,
- Parents may be focused on cancer treatment and their child’s immediate health.
- Parents may feel uncomfortable discussing issues of reproduction with their children.
Fertility Preservation - Where Does It Fit?
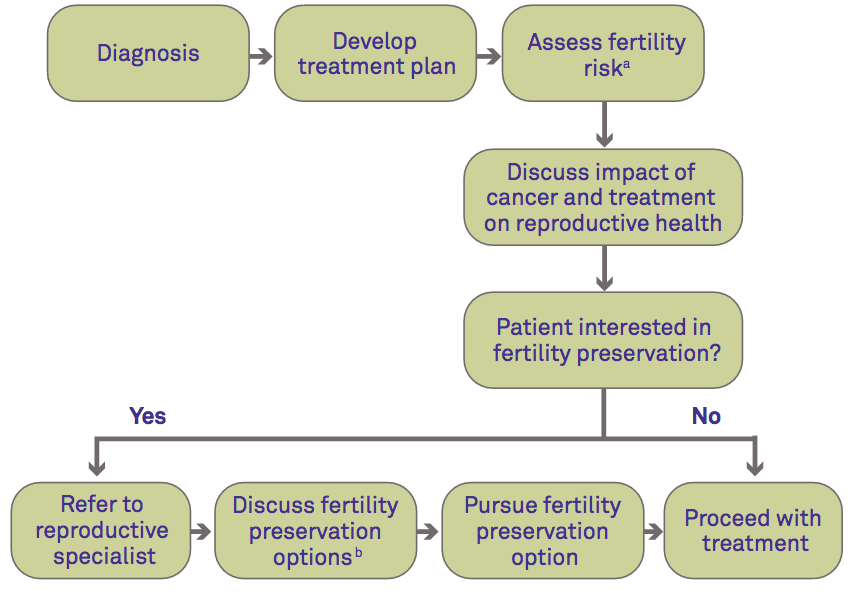
a) See table below
b) See figure below
Starting the Conversation
Discussing fertility preservation is important. These key points can help start the conversation:
- Cancer and cancer treatment may affect your child’s fertility.
- Based on your child’s treatment plan, his/her risk of infertility is [high, moderate, low] (see table on reverse).
- There are options to try to preserve your child’s fertility before he/she begins cancer treatment (see figure to right).
- I can refer you to a fertility preservation specialist if you would like to discuss your child’s options further.
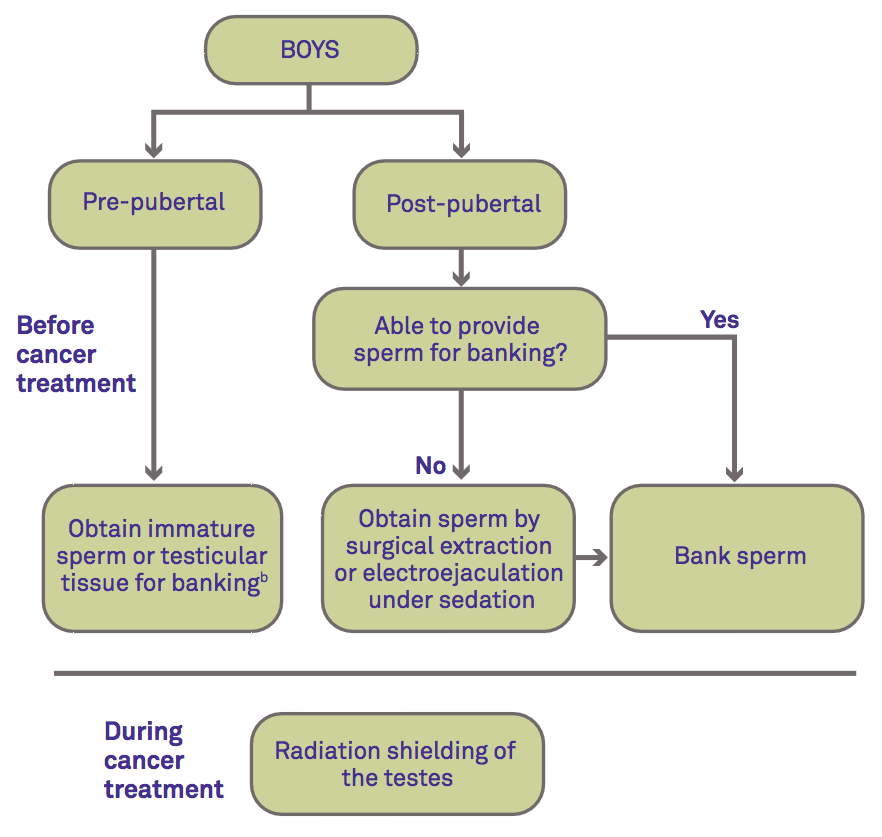
Options for Fertility Preservation
- The following diagram gives a brief description of fertility preservation options available to children diagnosed with cancer before and after treatment.
- There are several resources listed on the reverse that can help you and your patients locate a fertility preservation specialist to discuss tissue banking.
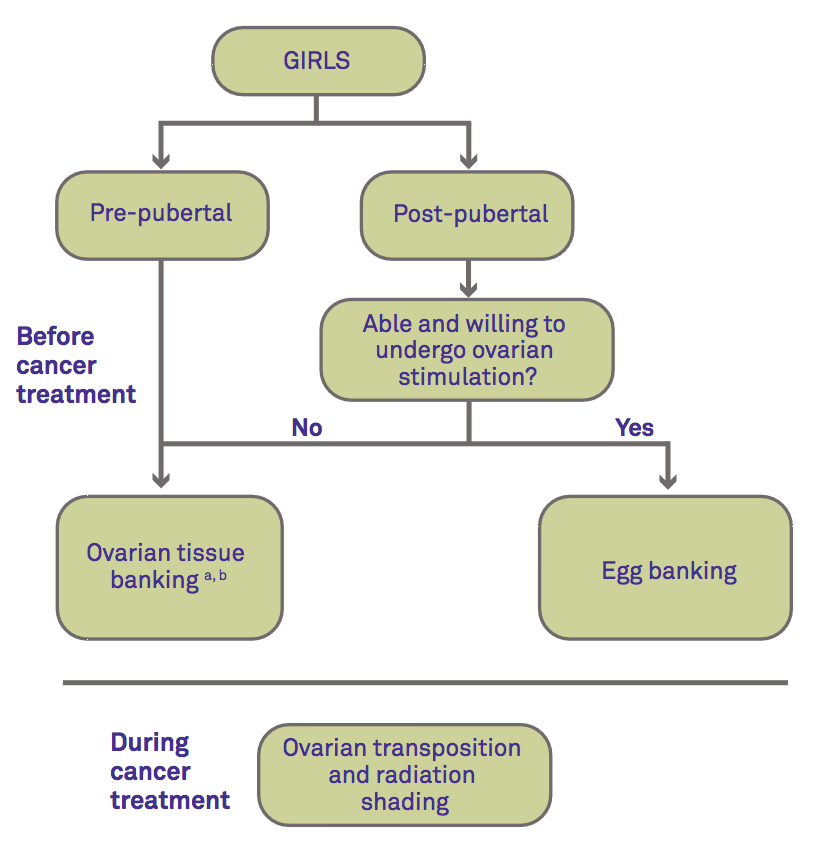
a Not an option if there is a high risk of ovarian metastases.
b Experimental—only performed as part of a clinical study approved by an IRB.
Cancer Therapy and the Risk of Infertility
The following table classifies various cancer therapies and regimens based on their known infertility risk. While this table provides general guidelines, each patient is different and treatment may impair their fertility differently.
| High Risk |
|
|---|---|
| Intermediate Risk |
|
| Low Risk |
|
| Very Low / No Risk |
|
| Unknown Risk |
|
Table adapted from LIVESTRONG; Nieman CL, et al. Cancer Treat Res. 2007;138:201-217; and Chow EJ, et al. Lancet Oncol. 2016;17:567-76.
Resources
For more information about infertility risk and fertility preservation options for children diagnosed with cancer:
- Visit SaveMyFertility.org
- Call the FERTLINE: 866-708-FERT (3378)
- Visit the Oncofertility Consortium Web site
- Use the online Clinic/Center Finder to find the fertility preservation center closest to you
- Visit the Pediatric Oncofertility Research Foundation
References
- The Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in patients facing gonadotoxic therapies: a committee opinion. Fertil Steril. 2013; 100:1224-31.
- Chow EJ, et al. Pregnancy after chemotherapy in male and female survivors of childhood cancer treated between 1970 and 1999: a report from the Childhood Cancer Survivor Study cohort. Lancet Oncol. 2016;17(5):567-76.
- Ginsberg JP. New advances in fertility preservation for pediatric cancer patients. Curr Opin Pediatr. 2010;23:9-13.
- Long CJ, Ginsberg JP, Kolon TF. Fertility Preservation in Children and Adolescents With Cancer. Urology. 2016;91:190-6.
- Loren AW, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013; 31: 2500-10.
- Nieman CL, et al. Fertility preservation and adolescent cancer patients: lessons from adult survivors of childhood cancer and their parents. Cancer Treat Res. 2007;138:201-217.
- Redig AJ, Brannigan R, Stryker SJ, et al. Incorporating fertility preservation into the care of young oncology patients. Cancer. 2010;117:4-10.

